BASICS
- Fructose consumption is linked to increased production of ‘bad’ or small dense LDL’s.
- LDL-C measures small ‘bad’ LDL’s and large ‘good’ LDL’s
- Polyunsaturated oils are significantly associated with increasing the oxidation and inflammatory process.
- Current cholesterol and lipid profile testing is misleading.
- The Triglyceride level is the MOST relevant and easily testable.
- Relevant other tests are Apolipoprotein A1, Apolipoprotein B and Lipid Subfraction analysis
_________________________
LIPID Testing Handout for you and your Doctor
DOWNLOAD What to expect when you move to LCHF – Low Carb and Healthy Fat Living – PDF 20160306
_________________________
The NoFructose Handout Starter Sheet is your take away summary of this web site. Read it at the NoFructose Starter Sheet area of this web site or download it.
IDEAS
Cutting down on Fructose consumption SHOULD decrease the production of the ‘bad’ small dense LDL’s and therefore minimise the load of inflammatory lipoproteins in to vessel walls and tissue.
There is no simple and cheap test for measuring small dense ‘bad’ LDL’s. We only measure it indirectly by LDL-C which has small ‘bad’ LDL’s and large ‘good’ LDL’s together.
The ratio of LDL-C and HDL-C is a very indirect assessment of risk. This is a measure of the cholesterol proportion of those lipoproteins.
An elevated cholesterol is probably meaningless in isolation.
Triglyceride levels reflect the circulating phospholipid profile. The lower the better. If your number is under 0.7 mmol/l or 62 mg/dL then you have very minimal ‘bad’ LDL’s in the circulation. Numbers above that reflect circulating inflammatory phospholipids.
Dietary changes and exercise will reduce triglyceride levels far more than any drug intervention.
Measuring actual particle numbers is the only way to go rather than ratios.
My recommendation is to test the following. It may cost a few hundred dollars but will be infinitely cheaper than embarking on a lifetime of statin cholesterol lowering drugs.
- Apolipoprotein A1 – a measurement of HDL particles
- Apolipoprotein B – a measurement of LDL particles
- Lipid Subfraction analysis – looks at the true spectrum size of Lipoproteins
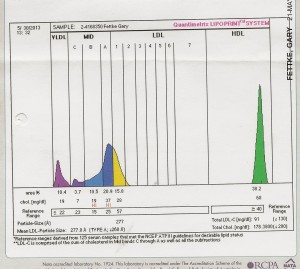
Here is my lipid subfraction analysis after going NoFructose. High HDL and Low LDL but importantly NO LDL particles in the 3 to 7 zones. These are the Small Dense LDL’s which are associated with cardiovascular disease.
TESTING
I regularly get asked as to where these ‘relevant’ tests can be performed. Ask your doctor.
Triglycerides are routine.
Apolipoprotein A1 and Apolipoprotein B measure the HDL and LDL particle number and should be easily available from pathology services.
The Lipid Subfraction analysis is done out of the Sydney Adventist Hospital Pathology. All labs can forward the test onto them.
SAN Pathology
185 Fox Valley Rd, Wahroonga NSW 2076
_____________________________
Professor Ken Sikaris on Blood Tests to Assess Cardiovascular Risk
https://www.youtube.com/watch?v=9BFRi-nH1v8&index=3&list=PLrVWtWmYRR2CSIwJs3jUpuwO7TLslIGpJ
______________________
 How do statins create their side effects?
How do statins create their side effects?
Statins provide only a small benefit of reducing your risk of dying from a heart attack if you have had a previous heart attack but they come at a cost. And that cost looks to be increasing. There is now increasing evidence of increased risks of diabetes, cancer, dementia, cataracts and musculoskeletal pain for those taking statin drugs.
Anything that reduces cholesterol production has far reaching consequences. Cholesterol is an integral part of our cell membranes, it holds us together. It makes up nearly 20% of our brains and it is integral to hormone production. If we keep affecting the building blocks of our cells then we have the potential to affect our long term health.
Most of the statin trials have been short term and tend to skip over the side effects. The benefits of reduction of risk sound a lot better when the drug companies push the relative risk reductions of these drugs rather than the actual numbers. A 1% absolute reduction from 3% doesn’t sound nearly as impressive as a 33% relative risk reduction. Guess what the drug companies push? It’s just statistics but… it’s also marketing. The long term studies are starting to look dubious when it comes to side effects…
http://www.nofructose.com/2015/08/14/statin-side-effects-or-lchf/#more-3008
________________________________
MORE INFORMATION
Cholesterol
Cholesterol is one of the most maligned substances I know. It is a form of alcohol. It does not dissolve in water and is a major component of our cell membrane wall. It holds us up!
It is not a fat and it is not in fact bad for us. The amount that we ingest has very little to do with the daily turnover of the cholesterol levels within our tissues.
It is a potent hormone precursor for estrogen and testosterone synthesis as well as being involved in our vitamin D synthesis. It is also required in scar tissue.
It was first measured in 1924 and has become a convenient indirect measure of a lipid profile. HDL-C and LDL-C are actually only measuring the cholesterol content in the lipoprotein rather than the actual amount of fat within them.
HDL-C / LDL-C ratios are very indirect measures.
The true level of Small LDL’s is not measured routinely. Apolipoprotein B can be measured which is a better predictor of cardiovascular disease.
The LDL pattern B of High levels of small dense LDL’s, low HDL and elevated triglycerides are not routinely measured. This is the bad combination.
Standard Lipid Profiles are Misleading
Dr. Thomas Dayspring, a lipidologist, has been saying all along that the standard Lipid Profile test that you get done at the doctor’s office is outdated and may not accurately predict atherogenic risk. Here is a video where he discusses lipid profiling and a case study that shows a dramatic turnaround by lifestyle changes – diet and exercise being the big changers that improved the lipid profile and decreased the risk of heart disease.
http://www.youtube.com/watch?feature=player_embedded&v=an6L9VY0v8A
Lipid Testing Summary
I have taken this transcript directly from a blog by Dr Chris Kresser. He is a nutritionist but it it is the best lay description that I have found on this topic.
The most important thing you probably don’t know about cholesterol
By Chris Kresser on January 20, 2010 in Food & Nutrition, Heart Disease, Myths & Truths
Summary:
- The simplified view of cholesterol as “good” (HDL) or “bad” (LDL) has contributed to the continuing heart disease epidemic
- Not all LDL cholesterol is created equal. Only small, dense LDL particles are associated with heart disease, whereas large, buoyant LDL are either benign or may protect against heart disease.
- Replacing saturated fats with carbohydrates – which has been recommended by the American Heart Association for decades – reduces HDL and increases small, dense LDL, both of which are associated with increased risk of heart disease.
- Dietary cholesterol has a negligible effect on total blood LDL cholesterol levels. However, eating eggs every day reduces small, dense LDL, which in turn reduces risk of heart disease.
- The best way to lower small, dense LDL and protect yourself from heart disease is to eat fewer carbs (not fat and cholesterol), exercise and lose weight.
Not all cholesterol is created equal
By now most people have been exposed to the idea of “good” and “bad” cholesterol. It’s yet another deeply ingrained cultural belief that has been relentlessly driven into our heads for several decades.
The oversimplified view of HDL cholesterol as “good” and LDL cholesterol as “bad” is not only incomplete, it has also directly contributed to the continuing heart disease epidemic worldwide.
But before we discover why, we first have to address another common misconception. LDL and HDL are not cholesterol. We refer to them as cholesterol, but they aren’t. LDL (low density lipoprotein) and HDL (high density lipoprotein) are proteins that transport cholesterol through the blood. Cholesterol, like all fats, doesn’t dissolve in water (or blood) so it must be transported through the blood by these lipoproteins. The names LDL and HDL refer to the different types of lipoproteins that transport cholesterol.
In addition to cholesterol, lipoproteins carry three fat molecules (polyunsaturated, monounsaturated, saturated – otherwise known as a triglyceride). Cholesterol is a waxy fat particle that almost every cell in the body synthesizes, which should give you some clue about its importance for physiological function.
You do not have a cholesterol level in your blood, because there is no cholesterol in the blood. When we speak of our “cholesterol levels”, what is actually being measured is the level of various lipoproteins (like LDL and HDL).
The consensus belief, as I’m sure you’re aware, is that LDL is “bad” cholesterol and HDL is “good” cholesterol. High levels of LDL put us at risk for heart disease, and low levels of LDL protect us from it. Likewise, low levels of HDL are a risk factor for heart disease, and high levels are protective.
It’s such a simple explanation, and it helps drug companies to sell more than $14 billion dollars worth of “bad” cholesterol-lowering medications to more than 24 million Americans each year.
The only problem (for people who actually take the drugs, rather than sell them, that is) is the idea that all LDL cholesterol is “bad” is simply not true.
In order for cholesterol-carrying lipoproteins to cause disease, they have to damage the wall of an artery. The smaller an LDL particle is, the more likely it is to do this. In fact, a 1988 study showed that small, dense LDL are three times more likely to cause heart disease than normal LDL.
On the other hand, large LDL are buoyant and easily move through the circulatory system without damaging the arteries.
Think of it this way. Small, dense LDL are like BBs. Large, buoyant LDL are like beach balls. If you throw a beach ball at a window, nothing happens. But if you shoot that window with a BB gun, it breaks.
Another problem with small LDL is that they are more susceptible to oxidation. Oxidized LDL, or oxLDL, is formed when the fats in LDL particles react with oxidation and break down.
Researchers have shown that the smaller and denser LDL gets, the more quickly it oxidizes when they subject it to oxidants in a test tube.
Why does this matter? oxLDL is a far greater risk factor for heart disease than normal LDL. A large prospective study by Meisinger et al. showed that participants with high oxLDL had more than four times the risk of a heart attack than patients with lower oxLDL.
I hope it’s clear by now that the notion of “good” and “bad” cholesterol is misleading and incomplete. Not all LDL cholesterol is the same. Large, buoyant LDL are benign or protect against heart disease, whereas small, dense LDL are a significant risk factor. If there is truly a “bad” cholesterol, it is small LDL. But calling all LDL “bad” is a dangerous mistake.
Low-fat, high-carb diets raise “bad” cholesterol and lower “good” cholesterol
Here’s where the story gets even more interesting. And tragic.
Researchers working in this area have defined what they call Pattern A and Pattern B. Pattern A is when small, dense LDL is low, large, buoyant LDL is high, and HDL is high. Pattern B is when small, dense LDL is high, HDL is low, and triglycerides are high. Pattern B is strongly associated with increased risk of heart disease, whereas Pattern A is not.
It is not saturated fat or cholesterol that increases the amount of small, dense LDL we have in our blood. It’s carbohydrate.
Dr. Ronald Krauss has shown that reducing saturated fat and increasing carbohydrate intake shifts Pattern A to Pattern B – and in the process significantly increases your risk of heart disease. Ironically, this is exactly what the American Heart Association and other similar organizations have been recommending for decades.
In Dr. Krauss’s study, participants who ate the most saturated fat had the largest LDL, and vice versa.
Krauss also tested the effect of his dietary intervention on HDL (so-called “good” cholesterol). Studies have found that the largest HDL particles, HDL2b, provide the greatest protective effect against heart disease.
Guess what? Compared to diets high in both total and saturated fat, low-fat, high-carbohydrate diets decreased HDL2b levels. In yet another blow to the American Heart Association’s recommendations, Berglund et al. showed that using their suggested low-fat diet reduced HDL2b in men and women of diverse racial backgrounds.
Here’s what the authors said about their results:
The results indicate that dietary changes suggested to be prudent for a large segment of the population will primarily affect [i.e., reduce] the concentrations of the most prominent antiatherogenic [anti-heart attack] HDL subpopulation.
Translation: following the advice of the American Heart Association is hazardous to your health.
Eating cholesterol reduces small LDL
The amount of cholesterol in the diet is only weakly correlated with blood cholesterol levels. A recent review of the scientific literature published in Current Opinion in Clinical Nutrition and Metabolic Care clearly indicates that egg consumption has no discernible impact on blood cholesterol levels in 70% of the population. In the other 30% of the population (termed “hyperresponders”), eggs do increase both circulating LDL and HDL cholesterol.
Why is this? Cholesterol is such an important substance that its production is tightly regulated by the body. When you eat more, the body produces less, and vice versa. This is why the amount of cholesterol you eat has little – if any – impact on the cholesterol levels in your blood.
Eating cholesterol is not only harmless, it’s beneficial. In fact, one of the best ways to lower small, dense LDL is to eat eggs every day! Yes, you read that correctly. University of Connecticut researchers recently found that people who ate three whole eggs a day for 12 weeks dropped their small-LDL levels by an average of 18 percent.
If you’re confused right now I certainly don’t blame you.
Let’s review what we’ve been told for more than 50 years:
- Eating saturated fat and cholesterol in the diet raises “bad” cholesterol in the blood and increases the risk of heart disease.
- Reducing intake or saturated fat and cholesterol protects us against heart disease.
Now, let’s examine what credible scientific research published in major peer-reviewed journals in the last decade tells us:
- Eating saturated fat and cholesterol reduces the type of cholesterol associated with heart disease.
- Replacing saturated fat and cholesterol with carbohydrates lowers “good” (HDL) cholesterol, raises triglyceride levels, and increases our risk of heart disease.
Dr. Krauss, the author of one of the studies I mentioned above, recently said in an interview published in Men’s Health, “Everybody I know in the field — everybody — recognized that a simple low-fat message was a mistake.”
In other words, the advice we’ve been given by medical “authorities” over the past half century on how to prevent heart disease is actually causing it.
I don’t know about you, but that makes me very angry. Heart disease is the #1 cause of death in the US. Almost 4 in 10 people who die each year die of heart disease. It directly affects over 80 million Americans each year, and indirectly affects millions more.
We spend almost half a trillion dollars treating heart disease each year. To put this in perspective, the United Nations has estimated that ending world hunger would cost just $195 billion.
Yet in spite of all this money spent, the best medical authorities can do is tell us the exact opposite of what we should be doing? And they continue to give us the wrong information even though researchers have known that it’s wrong for at least the past fifteen years?
____________________________
Good foods high in cholesterol.

https://authoritynutrition.com/7-healthy-high-cholesterol-foods/
___________________________
Please add information by going to Contribute to NoFructose.com
ARTICLES
Linoleic oil poly increases heart disease bmj.e8707.full
Polyunsaturated oil consumption increases cardiovascular events
Increased egg consumption protects against cardiovascular events
The Role of Triglycerides in Atherosclerosis
Current Cardiology Reports. 2011 December ; 13(6): 544–552. doi:10.1007/s11886-011-0220-3
Beatriz G. Talayero, MD, Frank M. Sacks, MD
Summary
Hypertriglyceridemia is a prevalent risk factor for cardiovascular disease (CVD) and increasingly
important in the setting of current obesity and insulin resistance epidemics. High triglyceride (TG)
levels are markers for several types of atherogenic lipoproteins. Patients who have
hypertriglyceridemia may be at significant risk for CVD even if low-density lipoprotein
cholesterol levels are at goal, and therefore warrant treatment that optimizes diet, reduces
overweight, and promotes regular exercise. High-risk patients with hypertriglyceridemia, such as
those with diabetes, CVD, or metabolic syndrome, may benefit from additional drug treatment
aside from a statin to address other lipid abnormalities. In this discussion, we review the role of
hypertriglyceridemia and its associated atherogenic lipoproteins in the pathogenesis of
atherosclerosis, the relevance of a high TG level as a predictor of CVD, the cardiovascular
outcomes from TG-lowering intervention trials, and the current guidelines for treating
hypertriglyceridemia.
Understanding_the_Entire_Lipid_Profile
Low Density Lipoproteins Containing Apolipoprotein C-III and the Risk of Coronary Heart Disease
Circulation. 2011 November 8; 124(19): 2065–2072.
doi:10.1161/CIRCULATIONAHA.111.056986.
Carlos O Mendivil, MD, DSc, Eric B. Rimm, DSc, Jeremy Furtado, DSc, Frank M Sacks, MD
Summary
LDL that contains apolipoprotein C-III (apoC-III) comprises only 10 to 20% of plasma LDL, but has a markedly altered metabolism and proatherogenic effects on vascular cells.
Concentrations of LDL with apoC-III (measured as apoB in this fraction) were associated with
risk of CHD in multivariable analysis that included the total cholesterol to HDL cholesterol ratio,
LDL cholesterol, apolipoprotein B, triglycerides, or HDL cholesterol; and other risk factors. In all
models, the relative risks for the top versus bottom quintile of LDL with apoC-III were greater
than those for LDL without apoC-III.
Conclusions—The risk of CHD contributed by LDL appeared to result to a large extent from LDL that contains apoC-III (measured in the Apolipo B number)
Novel biological functions of high-density lipoprotein cholesterol.
Mineo C, Shaul PW. Circulation Research 2012 Sep 28;111(8):1079-90.
Abstract
In addition to its role in reverse cholesterol transport, high-density lipoprotein (HDL) cholesterol has direct action on numerous cell types that influence cardiovascular and metabolic health. Cellular responses to HDL entail its capacity to invoke cholesterol efflux that causes signal initiation via scavenger receptor class B, type I, and plasma membrane receptor activation by HDL cargo molecules. In endothelial cells and their progenitors, HDL attenuates apoptosis and stimulates proliferation and migration. HDL also has diverse anti-inflammatory actions in both endothelial cells and leukocytes. In vascular smooth muscles, HDL tempers proinflammatory, promigratory, and degradative processes, and through actions on endothelium and platelets HDL is antithrombotic. There are additional actions of HDL of potential cardiovascular consequence that are indirect, including the capacities to promote pancreatic β-cell insulin secretion, to protect pancreatic β cells from apoptosis, and to enhance glucose uptake by skeletal muscle myocytes. Furthermore, HDL decreases white adipose tissue mass, increases energy expenditure, and promotes the production of adipose-derived cytokine adiponectin that has its own vascular-protective properties. Many of these numerous actions of HDL have been observed not only in cell culture and animal models but also in human studies, and assessments of these functions are now being applied to patient populations to better-elucidate which actions of HDL may contribute to its cardioprotective potential and how they can be quantified and targeted. Further work on the many mechanisms of HDL action promises to reveal new prophylactic and therapeutic strategies to optimize both cardiovascular and metabolic health.
Low-density lipoprotein particle number predicts coronary artery calcification in asymptomatic adults at intermediate risk of cardiovascular disease.
Abstract
BACKGROUND:
Clinicians require more discriminating measures of cardiovascular risk than those currently used in most clinical settings. A promising avenue of research concerns the relationship of low-density lipoprotein (LDL) subfractions to subclinical atherosclerosis.
To assess cross-sectional associations between subfractions of LDL cholesterol and coronary artery calcification (CAC).
The study sample comprised 284 asymptomatic clinic patients who were at intermediate risk of cardiovascular disease, aged 40-69 years, who were not taking a statin or niacin. Lipoprotein subclass measures were obtained by the use of proton nuclear magnetic resonance spectroscopy. CAC was assessed with computed tomography angiography (CTA). The analyses modeled the presence or absence of CAC.
RESULTS:
Total LDL particle number (LDL-P) had a stronger association with CAC than the traditional lipoprotein measures. Patients in the highest tercile of total LDL-P (1935-3560 nmol/L) were 3.7 times more likely to exhibit coronary artery calcification as those in the lowest tercile (620-1530 nmol/L). The independent effects of small LDL-P remained significant after adjustment for LDL-cholesterol, high-density lipoprotein (HDL), triglycerides, non-HDL, and large LDL-P. HDL and non-HDL were not significant, independent predictors of CAC.
CONCLUSION: Small LDL-P was a strong, independent predictor of the presence of CAC. Large prospective studies are needed to examine the effect of LDL particle number and size on coronary artery calcification.
More to follow