BASICS Fructose Metabolism
- As Hunter Gatherers we have a primitive survival instinct for finding sweetness in foods.
- Elegant Fructose (1/2 of Sugar) metabolism to support that primitive addiction.
- Small intestine absorption via GLUT 5 gut receptors.
- Upregulation number of GLUT 5 gut receptors within 24 hours to allow greater Fructose absorption (ability to increase metabolism at time of plenty).
- Down regulate GLUT 5 gut receptors with starvation.
- Almost exclusive Liver absorption via GLUT 2 receptors.
- Liver metabolism
- Fatty acid production to VLDL’s and then LDL’s to Fat storage – Obesity.
- Appetite stimulation by inhibition of Insulin and Leptin at the hypothalamus (satiety centre) and stimulates Ghrelin at stomach.
- Uric acid production.
- Aldehyde (alcohol production) pathway.
- Feedback mechanism to create tissue Insulin resistance via IRS-1 (insulin receptor substrate-1).
BASICS Fat Metabolism
- Fat is insoluble.
- Circulating fat is transported by Lipoproteins which vary in size and density.
- The proportions of Saturated, Monounsaturated and Polyunsaturated Fat in the lipoproteins and ultimately in all tissue is more dependent on what is ingested rather than produced.
- Polyunsaturated fat chains will be oxidised more than Saturated fat chains.
Hunter Gatherers for the last few hundred thousand years (whether or not us humans or apes) have been essentially programmed for food scarcity. We are constantly alert looking for food which leads to a heightened level of awareness. That survival instinct makes us intimately aware to look for sweetness in nature.
The fruit available at the end of Summer makes us immediately attracted to it and it is a survival mechanism. A tribal clan would have known where fruit trees are in their local environment and would have made that a significant destination at the time of Summer harvest. At the same time other animals right through to insects would be in the same environment and competition for this food source would have been significant.
The fructose metabolism pathway is elegant for making the most of that short term situation with a variety of mechanisms. The first is the immediate attraction to the fruit with both visual and taste stimuli.
There is a fairly immediate ability to encourage eating and gorging and then there is a subsequent up regulation of GLUT 5 receptors in the small intestine to allow the transport of Fructose in to the blood circulation. It is virtually all taken up by the liver and then metabolised within the liver effectively in to fat for Winter hibernation.
The fat is then transported as Lipoproteins to the organs of the body. The size of the particle vary but a significant proportion end up as Low Density Lipoproteins (LDL’s) which are just the right ‘Goldilocks’ size to create damage in the subintimal layer of every blood vessel wall.
The fat carried in this process is dependent on the fat ingested – a combination of Saturated, Monounsaturated and Polyunsaturated Oils. The greater the flexibility of the fat (more polyunsaturated), the greater the potential for oxidation and subsequent inflammation and tissue damage.
IDEAS
The consumption of Sugar and Polyunsaturated Seed Oils combine in our diet to create inflammation in every blood vessel wall and in every tissue in every organ of the body. The inflammatory process makes everything susceptible to damage and disease.
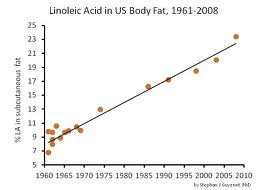
The main determinant of the proportion of Saturated, Monounsaturated and Polyunsaturated fats within our circulating lipoproteins and within tissue fat stores is the same as our diet. The western, modern diet has changed to a greater portion of Polyunsaturated fats over the last 50 to 100 years and this is reflected in the tissue accumulation of this component.
Read about the Damage Process
MORE INFORMATION
Sucrose (sugar) is rapidly cleaved in to Glucose and Fructose. Other combined sources of Fructose such as High Fructose Corn Syrup (HFCS), fruit or honey undergo the same rapid cleavage.
Glucose
- Glucose is a basic fuel, but ketones can be substituted.
- It is readily absorbed along the upper gut and then…
- Prioritised to the Brain, Muscles and then Cells of the body.
- Excess goes to the liver and is involved in Glycogen replenishment
- Any further excess goes to Fatty Acid production and this is processed in to Fat storage
- The Glucose effect on the pancreas promotes secretion of Insulin which acts on the Hypothalamus as a satiety agent (makes you less hungry)
Fructose
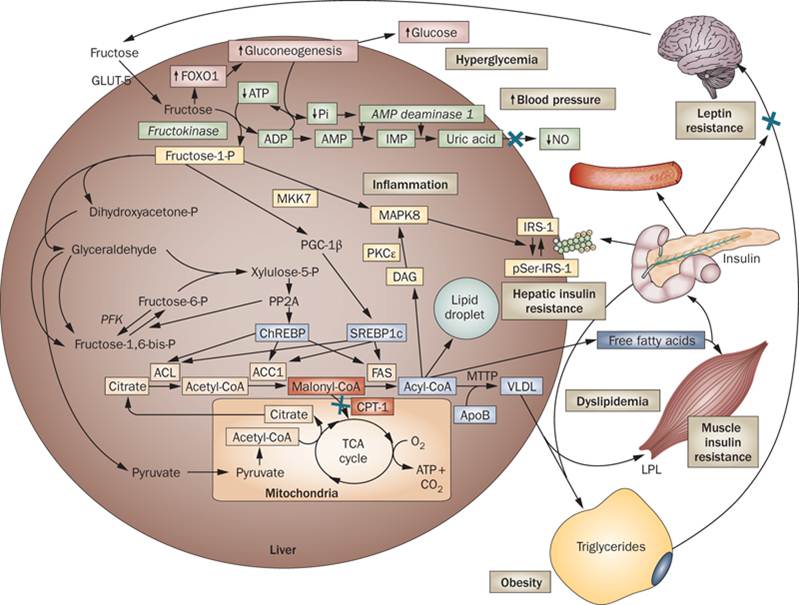
This fairly complex diagram is a reasonable summary of what happens in the liver to Fructose.
A small amount of Fructose goes via gluconeogenesis (upper tan pathway) to the immediate production of Glucose. In our current ingestion profile of Sucrose, the Glucose component is normally satisfied straight from the Sucrose and Fructose conversion to Glucose is negligible.
The green pathway is related to the phosphorylation of Fructose and the by-product of this is Uric Acid. This Uric Acid ultimately has an inhibitory effect on Nitric Oxide, which is a potent vasodilator in every blood vessel in the body.
Down to the left is an aldehyde pathway, which is the same concept as producing alcohol. In the outside world we ferment fruit to make alcohol and the liver does the same thing via a Fructose pathway. The aldehyde effects on the liver mean inflammation can occur within the liver.
The alcohol production within the substrate causes a cross linkage of proteins and its own low-grade inflammation. Over time this can result in fibrosis and the ultimate situation of cirrhosis and liver failure.
The yellow pathway leads to the production of IRS-1 (insulin receptor substrate-1), which is an important chemical in the feedback mechanism of insulin and the pancreas. Literature supports the fact that when fructose levels go up it has been associated with impaired intracellular insulin signalling and may be a factor in the pathophysiology of Type 2 diabetes mellitus.
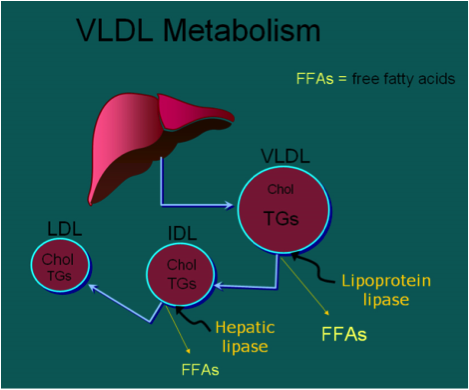
The blue pathway effectively shows the conversion of fructose into very low-density lipoproteins (VLDL’s), which are then discharged from the liver and combined with triglycerides to be transported around the body as fat stores.
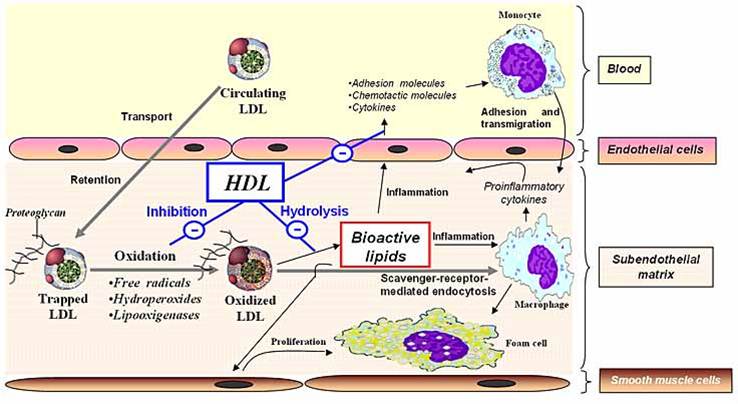
The green diagram above reveals that the VLDLs are then ultimately converted into LDLs in the transport around the body. These LDLs are what I describe as the ‘Goldilocks’ size for getting into the subintimal layer of the blood vessel walls between the endothelium and the smooth muscle walls.
The LDLs then sit within the vessel walls and, depending on the amount of saturated and polyunsaturated fat within it, then undergo an oxidation process.
If there is predominantly saturated fat then there is very little oxidation that occurs. The greater the proportion of polyunsaturated oils the greater the oxidation, inflammation and development of foam cells, which are those noted in the development of atherosclerotic plaque.
The other lipoproteins, which are then transported around the body and stored, undergo the same oxidative process in each organ where they end up. Again, the amount of oxidation is dependent on the component of poyunsaturated fat within them.
There has been an increased intake of polyunsaturated fat as a component of diet over the last 50 years and the following diagram reveals that the amount of linoleic acid, which is a polyunsaturated fat, within tissues has increased three-fold in the same time frame. This is clearly of concern because there is a far greater oxidation now occurring in 23 percent of the body tissue rather than the original 8 percent 50 years ago.
Clearly the whole process is a lot more complicated at a specific tissue and biochemical level but this is as close to a lay interpretation I can give.
Fructose is phosphorylated to Fructose-1-phosphate in the liver. The phosphate molecule required comes from a depletion of Adenosine triphosphate (ATP).
ATP is a molecule involved in energy transfer within cells. The phosphate within it is depleted when fructose is metabolised to fructose-1-phosphate by fructokinase. As a result of this depletion of energy stores within tissue, it acts like a form of ischemia with a transient arrest of protein synthesis and further oxidative stress within tissue. It has been associated with the production of inflammatory proteins and the combination of damage within the tissue, inflammatory proteins may be an issue for the modelling of disease within tissue.
The by-product of this breakdown is Uric Acid.
Uric Acid is distributed around the entire body and is excreted largely via the kidneys.
Nitric Oxide
Uric Acid has a potent inhibitory effect on Nitric Oxide Synthase which in turns affects Nitric Oxide activity.
There are three main forms of Nitric Oxide Synthase. They all act as Endothelium-Derived Relaxing Factor (EDRF) and have a vasodilatory effect through their action in the production of Nitric Oxide.
eNOS (endothelial Nitric Oxide Synthase)
- Acts on blood vessel endothelium
iNOS (inducible Nitric Oxide Synthase)
- Acts on white cells involved in immunity and tissue damage homeostasis
- Phagocytes
- Neutrophils
- Macrophages
- Monocytes
nNOS (neuronal Nitric Oxide Synthase)
- Acts on the brain and may be involved in the prioritisation of blood and oxygen supply to the brain.
The effect of Uric acid reducing Nitric Oxide bioavailability creates a variety of effects including
- Vasoconstriction and hypertension via its effect on vascular smooth muscle cells
- Oxidative stress in a variety of cells and particularly Adipocytes(fat cells)
- Endothelial cells permeability changes
- ? Immune effect by inhibiting phagocyte (white cell) activity
Fat Accumulation
The main determinant of the proportion of Saturated, Monounsaturated and Polyunsaturated fats within our circulating lipoproteins and within tissue fat stores is the same as our diet. The western, modern diet has changed to a greater portion of Polyunsaturated fats over the last 50 to 100 years and this is reflected in the tissue accumulation of this component.
What we eat is accumulated, transported and then stored. The lipoproteins are the transporters.
Read about the Damage Process
Read about the Health Issues
ARTICLES
Metabolic Effects of Fructose and the Worldwide Increase in Obesity
Luc TAPPY and Kim-Anne LE in PhysiologyReviews 90: 23–46, 2010; doi:10.1152/physrev.00019.2009.
While virtually absent in our diet a few hundred years ago, fructose has now become a major constituent of our modern diet. Our main sources of fructose are sucrose from beet or cane, high fructose corn syrup, fruits, and honey. Fructose has the same chemical formula as glucose (C6H12O6), but its metabolism differs markedly from that of glucose due to its almost complete hepatic extraction and rapid hepatic conversion into glucose, glycogen, lactate, and fat. Fructose was initially thought to be advisable for patients with diabetes due to its low glycemic index. However, chronically high consumption of fructose in rodents leads to hepatic and extrahepatic insulin resistance, obesity, type 2 diabetes mellitus, and high blood pressure. The evidence is less compelling in humans, but high fructose intake has indeed been shown to cause dyslipidemia and to impair hepatic insulin sensitivity. Hepatic de novo lipogenesis and lipotoxicity, oxidative stress, and hyperuricemia have all been proposed as mechanisms responsible for these adverse metabolic effects of fructose. Although there is compelling evidence that very high fructose intake can have deleterious metabolic effects in humans as in rodents, the role of fructose in the development of the current epidemic of metabolic disorders remains controversial.
Epidemiological studies show growing evidence that consumption of sweetened beverages (containing either sucrose or a mixture of glucose and fructose) is associated with a high energy intake, increased body weight, and the occurrence of metabolic and cardiovascular disorders.
Sugar, Uric Acid, and the Etiology of Diabetes and Obesity
RJ Johnson et al, Diabetes October 2013 vol. 62 no. 10 3307-3315
The intake of added sugars, such as from table sugar (sucrose) and high-fructose corn syrup has increased dramatically in the last hundred years and correlates closely with the rise in obesity, metabolic syndrome, and diabetes. Fructose is a major component of added sugars and is distinct from other sugars in its ability to cause intracellular ATP depletion, nucleotide turnover, and the generation of uric acid. In this article, we revisit the hypothesis that it is this unique aspect of fructose metabolism that accounts for why fructose intake increases the risk for metabolic syndrome. Recent studies show that fructose-induced uric acid generation causes mitochondrial oxidative stress that stimulates fat accumulation independent of excessive caloric intake. These studies challenge the long-standing dogma that “a calorie is just a calorie” and suggest that the metabolic effects of food may matter as much as its energy content. The discovery that fructose-mediated generation of uric acid may have a causal role in diabetes and obesity provides new insights into pathogenesis and therapies for this important disease.
___________________________________
Front Pharmacol. 2012; 3: 87.
Aldose Reductase, Oxidative Stress, and Diabetic Mellitus
More to follow.

 mmol/L), cellular glucose is predominantly phosphorylated into glucose 6-phosphate by hexokinase, and enters the glycolytic pathway. Only trace amounts of non-phosphorylated glucose (about 3%) enter the polyol pathway (Morrison et al.,
mmol/L), cellular glucose is predominantly phosphorylated into glucose 6-phosphate by hexokinase, and enters the glycolytic pathway. Only trace amounts of non-phosphorylated glucose (about 3%) enter the polyol pathway (Morrison et al.,